
The median postoperative echocardiography follow-up was shorter for patients who had the multipatch procedure but with one exception was longer than the latest detection of obstruction in the baffling or reimplantation group, and the difference did not reach statistical significance. There was no significant difference in the age at diagnosis or age at surgery in patients who had reimplantation or baffling compared with patients who had the multipatch technique. Demographic and clinical features are presented in Table 1. Of these patients, 4 had a baffling procedure, 7 had reimplantation, and 11 only had the new multipatch procedure. Twenty-two patients had surgery to redirect the scimitar vein at the IVC junction to the left atrium during the study period.
#Multipatch patching accepted format Patch#
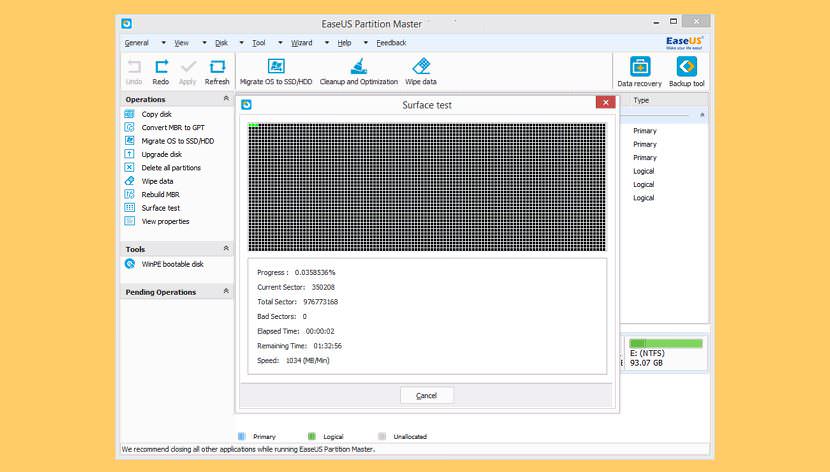
F, A pericardial patch is placed in the IVC in the region where the baffle patch was placed to “raise the roof” and augment the caliber of this region. The vena cava flow courses anterior to this patch ( blue arrows). E, An autologous pericardial patch is placed to divide the scimitar vein from the IVC and direct flow from the scimitar vein via a relatively straight baffle to the left atrium ( red arrows) effectively closing the atrial septal defect. D, A V-shaped incision is made in the atrium and scimitar vein and the space is filled in with a thin pulmonary homograft. The left atrium is pulled downward and anastomosed to the right atrial tissue bringing the left atrium closer to the scimitar vein. C, The atrial septum and superior limbic band have been resected. The atrial septum (1) and superior limbic band (2) are imaged. B, An incision is made in the right atrium and IVC to identify the origin of the scimitar vein. A, Baseline anatomy showing scimitar vein connecting to the IVC superior to the level of the diaphragm and intact atrial septum. The right atriotomy was closed, heart deaired, aortic crossclamp removed, patient warmed, and weaned from cardiopulmonary bypass.įigure 2 Triple patch operative technique to repair scimitar syndrome. The IVC was opened anteriorly down to the diaphragm and a third patch of autologous pericardium with running polypropylene suture was used to augment the IVC area where the atrial septation baffle patch had been placed ( Figure 2, F). Atrial septation was accomplished with a second patch of autologous pericardium that was sewn between the IVC and patched scimitar vein and carried up onto the superior limbus with running polypropylene suture completely closing the atrial septal defect and separating the IVC from the left atrium ( Figure 2, E). This avoids acute angle changes in the scimitar vein where it meets the lung parenchyma, where a fulcrum effect could lead to obstruction. The scimitar vein was not detached from the IVC to not change the angulation of the scimitar vein.
If the scimitar vein coursed adjacent to the left or right atrium, a V-shaped incision was made in the vein and the atrium was pulled down into this region and directly connected to the scimitar vein with running polypropylene suture without kinking or tension. A pulmonary homograft patch was chosen rather than a pericardial patch since it is more likely to conform to angles and not kink. This space was patch augmented with a thin pulmonary homograft with running polypropylene suture in an L-shaped fashion effectively enlarging the left atrium, taking any tension or torsion off the scimitar vein so as not to pull it too tightly to the left atrium, and shortening the scimitar pulmonary venous pathway. A right lateral atriotomy in the posterior part of the right atrium was made and opened down at a right angle into the scimitar vein creating a V-shaped incision ( Figure 2, D). The back wall of the left atrium was pulled rightward and downward toward the IVC to shorten the distance from the scimitar vein ( Figure 2, C, insert) and run together with interlocking polypropylene suture.
This resection included the back wall of the left atrium to that the heart was exited posteriorly. The atrial septum was fully resected critically removing the area of the muscular limbus ( Figure 2, B and C). If the scimitar vein was near the right atrial–IVC junction, an IVC cannula was placed inferiorly in a typical position if the scimitar vein entered at or below the diaphragm, an open-drop suction catheter was used. Cardiopulmonary bypass was established, cardioplegia administered, and diastolic arrest achieved. Autologous pericardium was harvested, fixed for 2 minutes in 0.6% glutaraldehyde, and rinsed.

The novel surgical technique incorporated a double- or triple-patch repair depending on the distance between the scimitar vein and atrial tissue ( Figures 2 and 3).


 0 kommentar(er)
0 kommentar(er)
